As women, it is never easy to hear that our physical health is compromised, especially when it comes to our reproductive system. For those who have been diagnosed with endometriosis, uncertainty about what comes next can feel overwhelming. Whether you’ve been diagnosed with endometriosis or you know someone who has, accurate information is key. The more informed you are on the topic, the more supported you will feel. In fact, understanding the causes, symptoms, and treatment options can provide you with a clear path forward.
What Is Endometriosis?
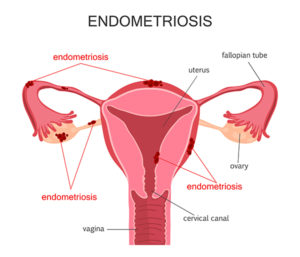
Endometriosis is a disorder in which tissue very much like the tissue that creates the lining of your uterus, known as the endometrium, develops in areas other than the uterus. Tissue growth can occur in areas it should not, including reproductive organs like the fallopian tubes and ovaries, as well as other pelvic tissue. Though uncommon, this tissue can even be found in areas outside the pelvic organs.
During endometriosis, the endometrial-like tissue takes on the functions and characteristics of your true endometrial tissue. As a result, the tissue will thicken, break down, and bleed during the menstrual cycle. The problem this presents is that there is no way for the tissue to exit your body. Normal pelvic tissue surrounding this foreign, trapped tissue can get inflamed and create scar tissue. Adhesions, which are bands of fibrous tissue, can develop and cause endometrial tissue that develops on organs to stick together. In addition, if tissue grows on the ovaries, cysts can form called endometriomas. Women with endometriosis can also experience severe pain during their menstrual cycle and could develop fertility issues.
Women with endometriosis may not notice the condition for some time, especially if they are prone to painful menstrual cramps or other discomforts. Eventually, however, most women do notice a significant difference in the severity of their menstrual pain, usually leading to a visit to their gynecologist. The good news is that once endometriosis is diagnosed, there are effective treatments available.
Endometriosis: Symptoms and Causes
Unfortunately, many women hesitate to explore medical concerns until they start to impact daily life, especially as they pertain to the reproductive system. A primary reason endometriosis so often goes undiagnosed is due to a delay in reaching out for healthcare. Fortunately, regular visits with your gynecologist can help you feel more comfortable opening up to your doctor and seeking treatment for any minor or major concerns.
If you’re concerned about a potential issue with your reproductive health, knowing the symptoms and causes of endometriosis can help you make the decision to seek treatment, understand the condition, and explore your treatment options.
Symptoms
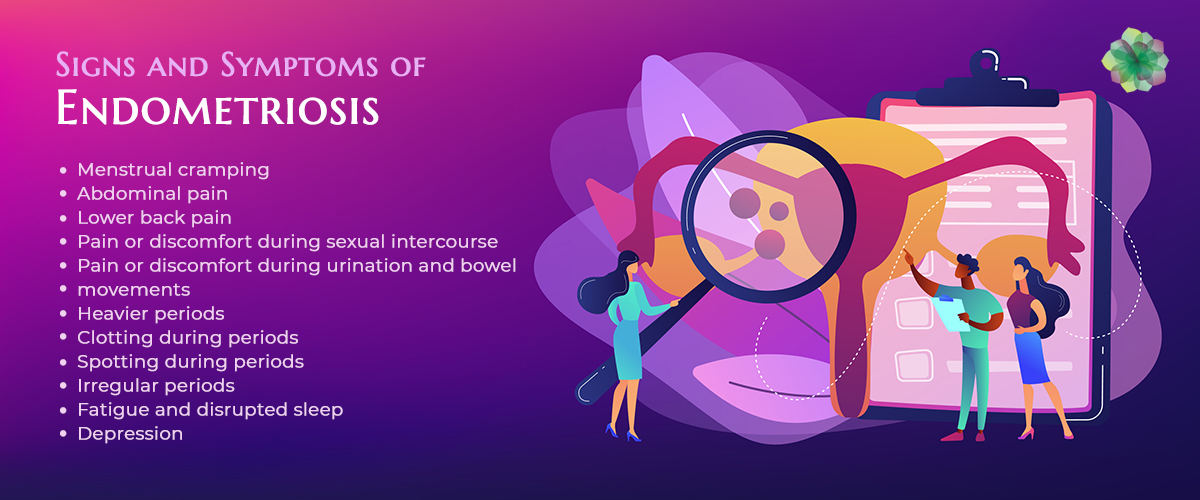
There are a variety of symptoms associated with endometriosis, the most common of which is pelvic pain that heightens during the menstrual cycle. The pain can be worse than usual and can also increase over time.
Other symptoms to look for include:
- Excessive Bleeding – Occasional heavy menstrual periods could occur, as well as bleeding between periods.
- Painful Periods – Also known as dysmenorrhea, pelvic pain and cramping could begin days before a menstrual cycle and continue to last for as long as 1-2 weeks. In addition to pelvic pain, you may also experience abdominal pain and lower back pain.
- Urinary and Bowel Pain – If you experience unusual pain while urinating or having a bowel movement, especially during a menstrual period, this could be an indicator of endometriosis.
- Pain with intercourse – A common symptom of endometriosis is pain during or after sex.
- Infertility – Endometriosis-related infertility is often detected when a woman seeks infertility treatment.
- Additional Symptoms – Endometriosis can also cause fatigue, nausea, constipation, bloating, or diarrhea.
It is beneficial to look for these additional symptoms beyond pelvic pain because while pelvic pain is often the reason many women discover their diagnosis, this symptom presents itself differently from case to case. Some women have mild endometriosis and experience severe pain, while others have advanced endometriosis with little to no pain. Everyone has a different pain tolerance, and the way endometriosis affects you can be drastically different compared to someone else.
Causes
There is still some uncertainty when it comes to the exact cause of endometriosis, and researchers have not identified a single cause that can trigger the condition. However, while the root cause is still uncertain, scientists have developed several theories.
Some possible explanations for endometriosis include:
- Transformation of peritoneal cells. Also known as “induction theory,” experts believe that hormones or immune factors may support the transformation of peritoneal cells into endometrial-like cells.
- Retrograde menstruation. In some cases, menstrual blood with endometrial tissue may continue on into the abdominal cavity via the fallopian tubes instead of being eliminated from the body. The cells may stick to the internal cavity walls and the associated organs, and with nowhere to go, this tissue could continue to build layers, thicken, and cause pain.
- Transformation of embryonic cells. Estrogen and other hormones can transform embryonic cells into endometrial-type cells during puberty, which can then implant into the abdominal cavity.
- Endometrial cell transport. Endometrial cells are transported to other parts of the body through blood vessels or tissue fluid and may wind up in the abdominal cavity.
- Surgical scar implantation. Endometrial cells may attach to a surgical incision, especially after surgeries involving the pelvic organs.
- Immune system issues. Immune disorders could also cause endometriosis. The body may be unable to identify and eliminate endometrial tissue developing in places it should not.
- Genetics. Family history may also play a role in your likelihood of developing this condition. Women who have a close relative with this condition are more prone to having it themselves.
What Are the Four Stages of Endometriosis?

If you or a loved one have recently received an endometriosis diagnosis, it is important to understand the four stages of endometriosis: minimal, mild, moderate, and severe. Understanding these stages can help you understand what to expect as you and your physician discuss treatment. There are a variety of factors used to determine the stage, including the location, number, size, and depth of the endometrial implants. It is beneficial to keep in mind that the pain you may experience during your menstrual cycle does not determine your endometriosis stage.
Stage One: Minimal
When a person is diagnosed with stage one or minimal endometriosis, the lesions caused by endometriosis are small, and the implants are shallow. Individuals with stage one may experience inflammation in the area.
Stage Two: Mild
Individuals with stage two endometriosis have mild lesions and endometrial tissue is implanted fairly shallow. This stage is considered mild endometriosis.
Stage Three: Moderate
Individuals who are in the moderate stage may have more lesions than seen in the previous stages. The endometriosis implants are typically deeper within both the pelvic lining and the ovaries.
Stage Four: Severe
Individuals in this stage likely have deep implants on both the ovaries and the pelvic lining. In many cases, there are lesions that could extend to the fallopian tubes and portions of the bowel region. There could also be cysts on one or both of the ovaries due to repetitive cycles of the endometriosis cells thickening, shedding, and becoming trapped.
The Diagnosis Process
Endometriosis can have similar symptoms to other conditions, including ovarian cysts, pelvic inflammatory disease, and even irritable bowel syndrome. This can prolong diagnosis and often requires a variety of tests to ensure accuracy. These delays can be significant; it can take some cases 4 to 11 years for a diagnosis from the onset of symptoms. Ongoing research and support are needed to ensure this timeframe can be significantly reduced so that accurate diagnosis can be given and the right treatment implemented. It can be frustrating, but patience and open communication with your healthcare team can help minimize the delay in proper diagnosis.
Things that are likely to occur during the diagnosis process include:
- A detailed medical history. Your doctor will likely explore any personal or family history of endometriosis, as there is an increased risk of developing endometriosis if a close family member also has the condition. Your doctor will complete a general health assessment to ensure your signs and symptoms aren’t connected to a different long-term disorder.
- A physical exam. Your doctor will complete a detailed pelvic examination to search for cysts or scars behind the uterus. A speculum and light will be used to see inside the vagina and cervix, helping the doctor determine the severity of your condition, as well as possibly rule out other conditions that may share other symptoms.
- Ultrasound imaging. A transvaginal or abdominal ultrasound can be used to provide clear images of your reproductive organs. An ultrasound helps identify cysts and lesions.
- Laparoscopic imaging. This is a minor surgical procedure that provides an opportunity to directly view endometriosis. Once a person is diagnosed with this condition, the same procedure can be used to remove the tissue.
Treatment Options

The main goal of endometriosis treatment is to alleviate pain and help you learn to cope with the physical and emotional challenges that can be associated with this condition. Which treatment is best for you will depend on your age, the severity of your symptoms, the severity of the condition itself, and any plans for future pregnancies. There are medications, alternative therapies, and surgeries that can be considered.
Medications
Medications can help you control the symptoms of endometriosis.
Hormonal options and medications include:
- Birth Control – Hormonal suppression can help reduce the symptoms associated with this condition, which can include using estrogen and progesterone birth control options such as oral birth control pills, patches, Nexplanon, IUD, a vaginal ring, or the birth control shot. These medications can help you experience less painful periods.
- GnRH Medications – Gonadotropin-releasing hormone medications stop the hormones associated with your menstrual cycle. This essentially puts your reproductive system on hold to help relieve pain.
- Danazol – Also known as Danocrine, this medication stops the production of hormones that cause a period. Individuals on this medication may have an occasional menstrual period, or they may stop entirely.
It is important to note that these medications are not recommended for those who are trying to get pregnant. In addition, if the medication is stopped in an attempt to become pregnant, endometriosis symptoms can come back. Your medical professional will discuss the details of these options with you. For pain relief, doctors commonly prescribe over-the-counter pain relief and non-steroidal anti-inflammatory drugs (NSAIDs) like acetaminophen and ibuprofen.
Surgery

Surgery can be an effective way to help relieve endometriosis pain and improve your ability to become pregnant. There are always risks associated with any form of surgery, so it is beneficial to discuss this treatment option with your provider. Endometriosis is a chronic disease, so surgery is not often the final solution. Symptoms may return within a few years, or they may not.
Surgical treatments include:
- Laparoscopy – This procedure can be used to diagnose and treat endometriosis. A surgeon makes a small cut into the abdomen and inserts a thin tube-like tool called a laparoscope into your body, which uses a high-definition camera to identify lesions so they can be accurately removed through the tube.
- Hysterectomy – In severe cases, removing the uterus may be suggested due to scar tissue and the extent of endometriosis in the pelvic area.
Alternative Therapies
Not everyone wants to turn to medications or surgery to experience relief. Some patients may experience symptom relief through holistic treatments and delay surgical procedures for a time.
These treatments may include:
- Acupuncture
- Herbal medication
- Dietary changes
- Pelvic floor muscle therapy
- Heat therapy
Endometriosis FAQs
Whether you have just received an endometriosis diagnosis or believe you may be experiencing symptoms of endometriosis, the answers to these common questions could shed some light on what to expect.
Can I Get Pregnant if I Have Endometriosis?
Endometriosis can make it more difficult to become pregnant, but pregnancy is not impossible. Your chances of becoming pregnant largely depend on the severity of your condition, as well as your treatment options. It may be recommended to try to conceive sooner than later, as this condition often worsens over time.
What Are the Risk Factors Associated with Endometriosis?
Common risk factors include a family history of endometriosis, when you started having your period, the length of your menstrual cycle, and any defects in your uterus or fallopian tubes. Having a close family member with the condition or menstruating before the age of 11 can increase your chances of developing endometriosis. Long menstrual cycles and uterine or fallopian tube defects can increase the chances that excess tissue will develop in the abdominal cavity.
Can Endometriosis Go Away on its Own?
Yes, in some cases. Lesions can get smaller, and you may only have a few of them. Menopause can also help alleviate or eliminate endometriosis since the body no longer produces estrogen. However, for most, this condition needs ongoing treatment to relieve pain and prevent the condition from worsening.
Let Us Support You
Endometriosis awareness can help individuals and their families better prepare and face this diagnosis. Currently, it can take years for an accurate endometriosis diagnosis, which can mean years of pain and discomfort that can only worsen over time. At Arizona Gynecology Consultants, women’s health is our top priority. We continue to strive for advancements in the diagnosis and treatment of this condition. View our Arizona gynecology services and book an appointment.
Editor’s Note: This article was originally published April 12, 2020 and was updated October 2, 2023.
References :
- Agarwal, S. K., Chapron, C., Giudice, L. C., Laufer, M. R., Leyland, N., Missmer, S. A., Singh, S. S., & Taylor, H. S. (2019). Clinical diagnosis of endometriosis: A call to action. American Journal of Obstetrics and Gynecology, 220(4), 354.e1–354.e12. https://doi.org/10.1016/j.ajog.2018.12.039
- ?Mayo Clinic. (2018, July 24). Endometriosis – Symptoms and Causes. Mayo Clinic; Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656
- Wadood, A. (2019, July 2). Endometriosis. Healthline; Healthline Media. https://www.healthline.com/health/endometriosis
- ?What are the symptoms of endometriosis? (n.d.). Https://Www.nichd.nih.gov/. https://www.nichd.nih.gov/health/topics/endometri/conditioninfo/symptoms
- ?Heitmann, R. J., Langan, K. L., Huang, R. R., Chow, G. E., & Burney, R. O. (2014). Premenstrual spotting of ?2 days is strongly associated with histologically confirmed endometriosis in women with infertility. American Journal of Obstetrics and Gynecology, 211(4), 358.e1–358.e6. https://doi.org/10.1016/j.ajog.2014.04.041
- ?Surrey, E. S., Soliman, A. M., Johnson, S. J., Davis, M., Castelli-Haley, J., & Snabes, M. C. (2018). Risk of Developing Comorbidities Among Women with Endometriosis: A Retrospective Matched Cohort Study. Journal of Women’s Health, 27(9), 1114–1123. https://doi.org/10.1089/jwh.2017.6432

Dr. Davitt followed his passion for medicine and surgery through his undergraduate training at Boston University and into medical school at Marshall University in West Virginia. Training in Obstetrics and Gynecology brought him back to his hometown of Washington D.C. where he completed residency at Georgetown University Hospital and Washington Hospital Center. After residency he pursued advanced surgical training through a fellowship in Minimally Invasive Gynecologic Surgery at the Mayo Clinic Hospital in Phoenix, AZ.







 When it comes to the risk of developing urinary incontinence, the chances vary drastically. Some symptoms of UI can point to larger issues that may need to be seriously addressed, while others may be milder and more temporary. The good news is that for most, these risks can be resolved quickly, leading to an only temporary risk of developing urinary incontinence. Risks can include:
When it comes to the risk of developing urinary incontinence, the chances vary drastically. Some symptoms of UI can point to larger issues that may need to be seriously addressed, while others may be milder and more temporary. The good news is that for most, these risks can be resolved quickly, leading to an only temporary risk of developing urinary incontinence. Risks can include: The good news is that not all these symptoms are long-term. Many are short-term and potentially treatable. There are some general symptoms, including vaginal infections, irritations, medication use, constipation, general mobility, and UTI (urinary tract infection) that are often common causes.
The good news is that not all these symptoms are long-term. Many are short-term and potentially treatable. There are some general symptoms, including vaginal infections, irritations, medication use, constipation, general mobility, and UTI (urinary tract infection) that are often common causes. Millions of Americans deal with some form of UI every day. This number is hard to measure due to the feeling of embarrassment that stops many from sharing their experience. The truth of the matter is that many people deal with various forms this condition may present itself in. Whether you feel you go to the bathroom too much, too little, or just too unexpectedly, there are various exercises and treatments that could help alleviate your symptoms. What matters most is your ability to be open and honest with your health care professional. You may feel you are alone, but in fact, you are with a great majority of people who experience similar issues. Break the silence and give yourself the opportunity to truly live life to its fullest. You should never feel chained to the restroom.
Millions of Americans deal with some form of UI every day. This number is hard to measure due to the feeling of embarrassment that stops many from sharing their experience. The truth of the matter is that many people deal with various forms this condition may present itself in. Whether you feel you go to the bathroom too much, too little, or just too unexpectedly, there are various exercises and treatments that could help alleviate your symptoms. What matters most is your ability to be open and honest with your health care professional. You may feel you are alone, but in fact, you are with a great majority of people who experience similar issues. Break the silence and give yourself the opportunity to truly live life to its fullest. You should never feel chained to the restroom.



 As mentioned above, when more women learn about all the types of birth control available to them, they tend to make different choices that better fit their lifestyles. Discussion regarding your reproductive health isn’t – and shouldn’t be – taboo. Learn about the different methods of birth control that may work for you, and after you make your choice, research the side effects, risks, and how to properly use them.
As mentioned above, when more women learn about all the types of birth control available to them, they tend to make different choices that better fit their lifestyles. Discussion regarding your reproductive health isn’t – and shouldn’t be – taboo. Learn about the different methods of birth control that may work for you, and after you make your choice, research the side effects, risks, and how to properly use them.
 Wende Scholzen, WHNP
Wende Scholzen, WHNP


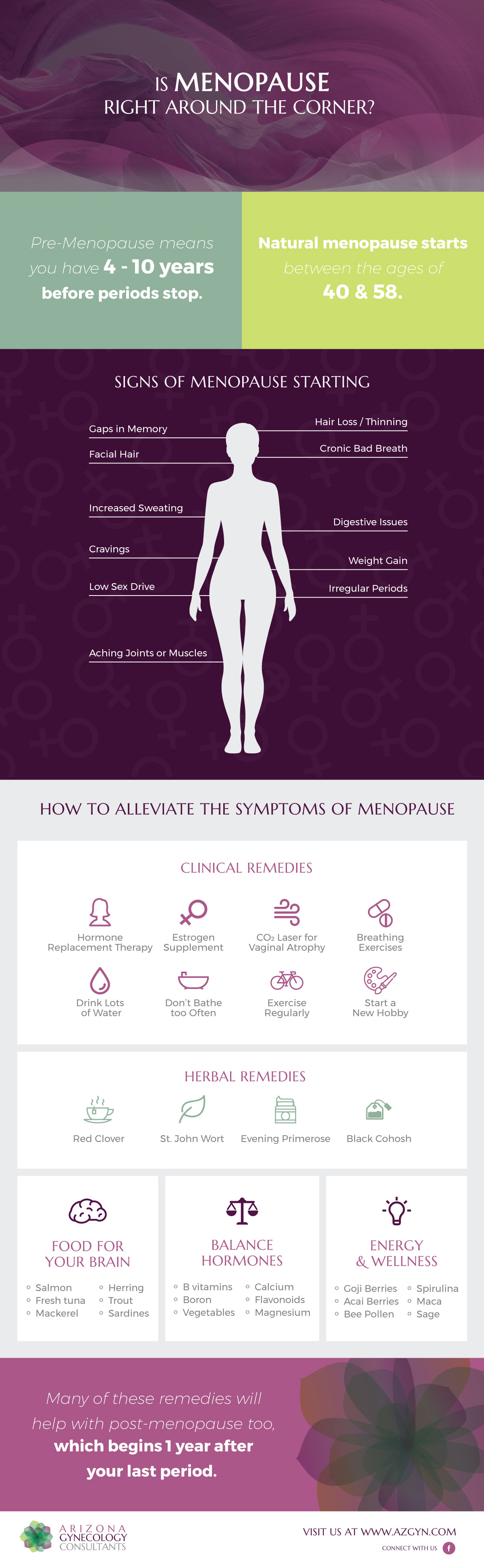
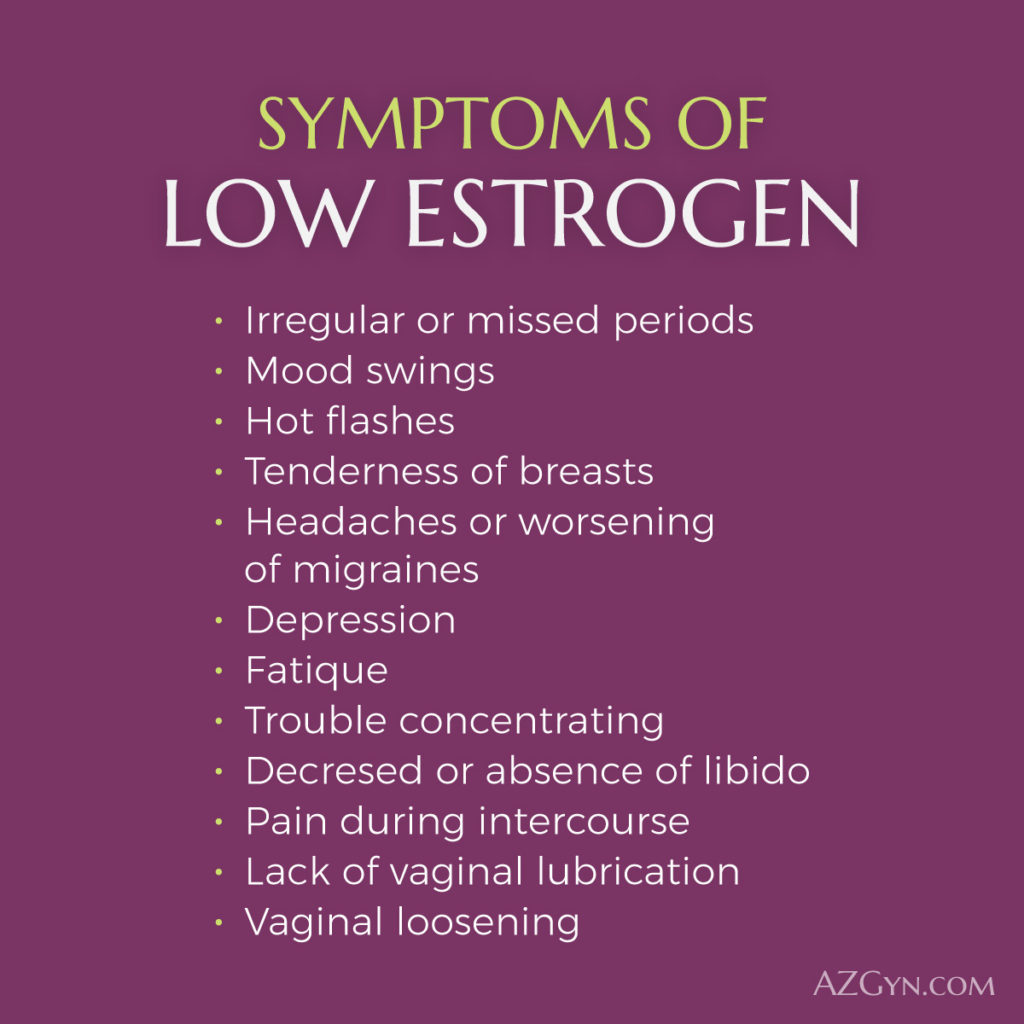
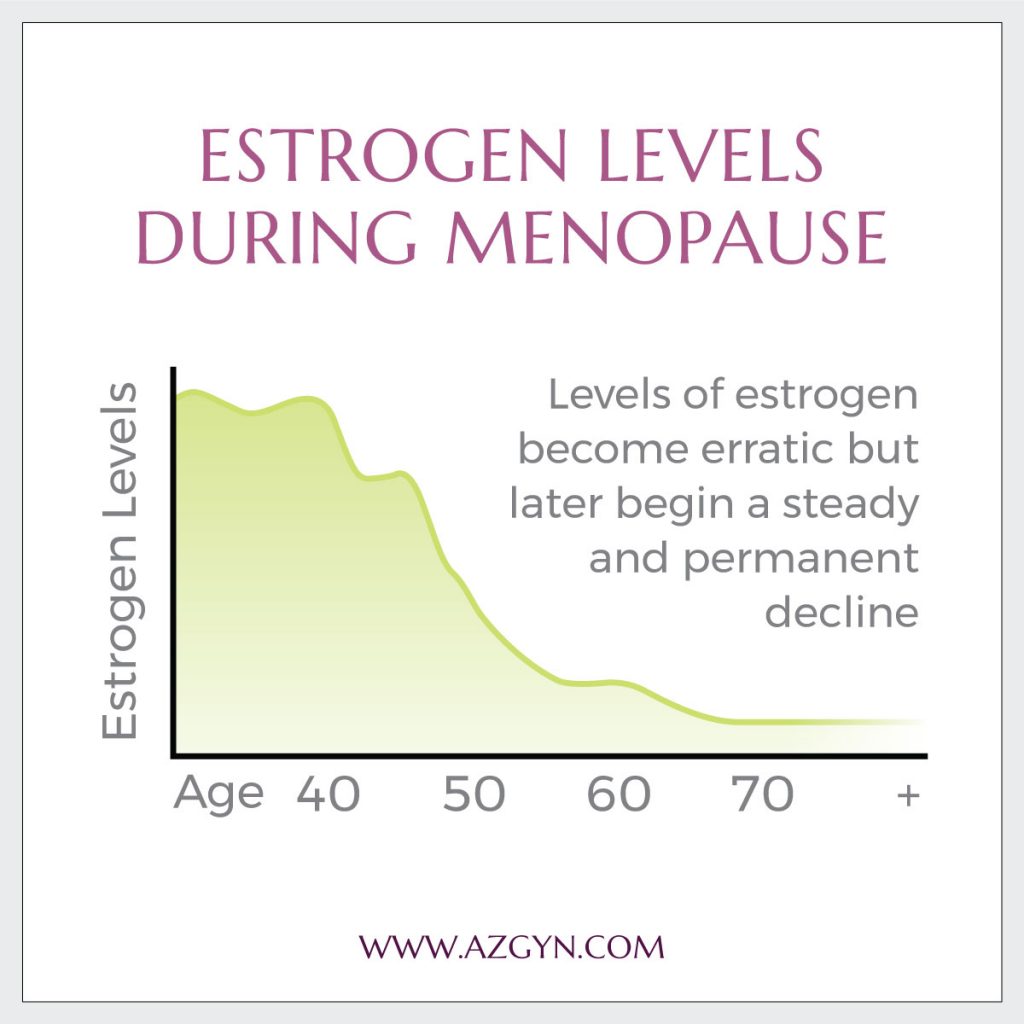 All women experience menopause, with several different symptoms.
All women experience menopause, with several different symptoms.
 According to the
According to the 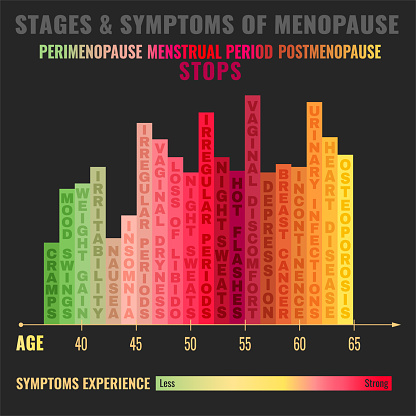

 While you are combating symptoms for an unknown period of time, look into common forms of relief. If you have medical conditions exacerbating the symptoms of menopause, such as arthritis, chronic pain, anxiety or depression, your doctor can help address these issues to potentially reduce menopause symptoms.
While you are combating symptoms for an unknown period of time, look into common forms of relief. If you have medical conditions exacerbating the symptoms of menopause, such as arthritis, chronic pain, anxiety or depression, your doctor can help address these issues to potentially reduce menopause symptoms.