It’s common for women to go years without any inkling of an issue with their reproductive health, only to experience difficulties when trying to conceive. While there are many avenues to exploring and treating infertility, the first question your doctor has may be regarding your diet. In fact, fertility specialists often recommend that you make adjustments to your diet, but this isn’t always related to your weight. Often, dietary changes are intended to help you improve your gut health, which has a unique relationship with fertility.
At Arizona Gynecology Consultants, we frequently work with women who are struggling to conceive. If this describes you, our compassionate team will take a thorough look at your overall health and help you make the changes necessary to increase your chances of pregnancy. Gut health is often overlooked when it comes to fertility, but by improving gut health for infertility, you, too, may be able to conceive. Get started by learning more about the link between fertility and gut health.
The Gut and Your Health
The gut consists of more than just your stomach. The gut is actually a long tube that begins at your mouth and travels through your esophagus, stomach, intestines, and finally, your anus. Supporting organs include the liver, kidneys, and pancreas. Anything you swallow, including food, drink, and medications, travels through your gut, where it is digested. Nutrients are absorbed through the gut lining and into the bloodstream to be processed into energy before the waste is expelled at the end.

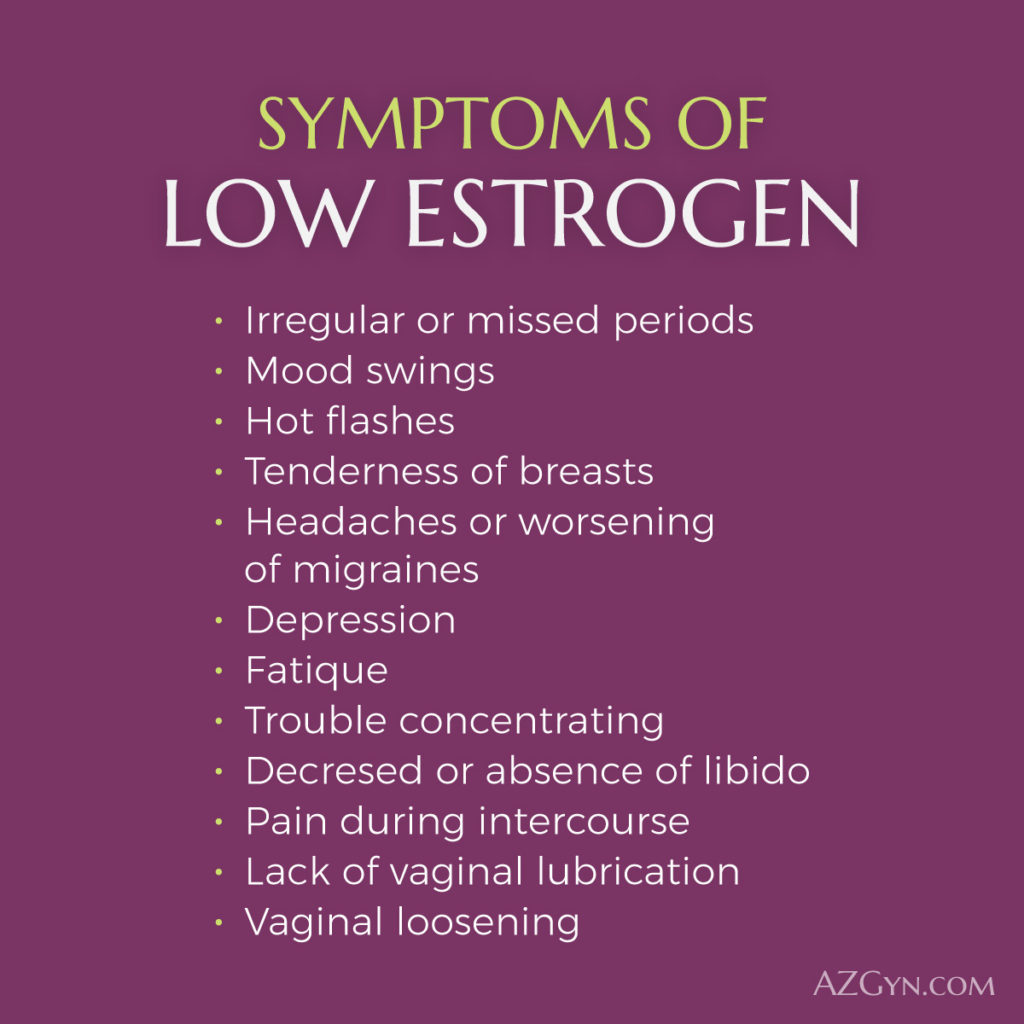
A crucial component of your gut includes microbes like the bacteria that populate your digestive system and particularly the large intestine. Microbes are responsible for aiding in gut movement, digesting foods, synthesizing and extracting vitamins and nutrients, and much more. Gut microbes also secrete an enzyme called glucuronidase, which allows estrogen to function properly throughout your body. A healthy microbiome, the collection of all the bacteria in your gut, can not only help you protect yourself from disease but also help you maintain your other bodily functions, including fertility.
How Can Your Gut Become Unhealthy?
There are several contributing factors that lead to an imbalanced gut:
Stress
Stress and anxiety can affect how your gut and brain interact with each other. Failure to conceive can be stressful, and your daily responsibilities and other stressors in your life can only make the problem more difficult to deal with. Worse, stress and impacts on the gut microbiota can cause serious disruptions in the chemical messengers responsible for maintaining important bodily functions, including gamete production, digestion, and more, causing a cycle of stress and physical issues. Stress can trigger symptoms in your gut by releasing stress hormones like cortisol, which directly interfere with gut microbiota. In turn, disruptions in gut microbiota can cause other conditions that increase stress.
Diet
Most women know just how essential it is to eat a healthy diet while pregnant, as the nutrients you consume can affect your child’s health long-term. However, diet is also just as important for your gut health, especially if you’re trying to conceive. Eating too much processed food, sugar, and other junk food can kill healthy bacteria in your gut, which are needed to ensure you are absorbing nutrients at the proper rate and producing the chemical messengers essential for all body functions.
Lack of Exercise
Exercise can be beneficial for both your physical and mental health. When you refrain from exercise, your gut becomes weaker, and you may even disrupt the delicate balance of microbes in your gut microbiota, making you more susceptible to various diseases and illnesses. Additionally, poor blood flow can prevent your gut from functioning optimally and inhibit your absorption of essential micronutrients for reproduction.
Alcohol
Drinking while trying to conceive can negatively affect your gut health, increasing your chances of infertility. For example, heavy drinking can lead to irregular periods, which can make it more difficult to conceive. Alcohol can also disrupt the gut microbiota, affecting the reproductive hormones so essential for conception and pregnancy.
How Fertility and Gut Health are Linked
There’s a link between fertility and gut health, and when your gut is unhealthy, you can experience problems with conception. In fact, gut imbalances can directly affect ovulation, ovary health, the fertilization process, the chances of implantation, and more. This occurs because the gut microbiome can be considered an endocrine organ in itself. It frequently interacts with sex hormones such as testosterone, androgen, estrogen, and estradiol, which support your reproductive health. Thus, when your gut health is compromised, the resulting sex hormone imbalances can lead to reproductive disorders or infertility.
An imbalanced gut microbiome can contribute to the following reproductive health conditions:
- Cancers
- Irregular Periods
- Vaginal Infections
- Polycystic ovary syndrome (PCOS)
- Endometriosis
It’s important to note that poor gut health doesn’t only affect women. In men, poor gut health can affect sperm quality, which can lead to a double dose of fertility difficulties. The microbiome can affect the body’s ability to produce sperm, which could affect his ability to conceive with you.
Gut Health and Pregnancy Complications
It’s important to remember that the importance of gut health doesn’t diminish once you conceive. In fact, poor gut health can cause issues with pregnancy and inhibit embryonic development. Researchers have revealed that the important “good” microbes in the gut are also present in the reproductive tract, including the vagina, uterus, and even the placenta that nourishes the fetus. As a result, disturbances in the gut microbiota can cause disruptions in the microbiota in the reproductive tract.

Issues with these two interlinked microbiomes can negatively affect the fetus’ developing microbiome and may continue to have an effect after the baby is born. In addition, disruptions can cause infections, affect placental health, inhibit fetal growth and development, and cause premature birth. Babies born to mothers with microbiome imbalances have lower birth weights and decreased survival rates.
How to Improve Gut Health
If you’ve been having trouble getting pregnant, you may be able to make lifestyle changes to improve your odds of pregnancy. One of the simplest changes involves addressing your diet and lifestyle for gut health. Consider consuming probiotic and prebiotic foods, limiting alcohol use, improving your exercise routine, and addressing both sleep and stress.
Eat Probiotic Foods
Probiotic foods contain microorganisms that improve gut health when ingested. They are typically created from fermented food in order to add “good” bacteria into the body. Fortunately, probiotic foods have existed for thousands of years and are readily available in your local supermarket.
Probiotic foods to consider incorporating into your diet include:
- Milk products such as yogurt, buttermilk, kefir, sour cream, and cheese
- Sauerkraut
- Kimchi
- Kombucha
- Miso
- Tempeh

The listed foods have been shown to positively influence the gut microbiome and benefit the rest of your health, as well. When improving gut health for infertility, you can also consider supplementing probiotics if you can’t eat foods with probiotics naturally included. However, because there are plenty of probiotic supplements available, it’s important to choose those that specifically address infertility. If you decide to supplement probiotics, talk to your doctor and our team at Arizona Gynecology Consultants to inform your decision.
Eat Prebiotic Foods
Prebiotic foods provide a non-digestible fiber that feeds your healthy gut microbes. If you ingest plenty of probiotics but neglect prebiotics, your probiotics won’t provide any meaningful effects.
Prebiotics are mostly found in plant-based foods, including:
- Oats
- Rye Bread
- Watermelon
- Garlic
- Asparagus
- Onions
- Chickpeas
To keep your gut in optimal health, consider incorporating the above foods into your diet. In doing so, your microbiome will remain healthy and able to process food and nutrients. Subsequently, you can take a prebiotic supplement if necessary. Both prebiotic and probiotic supplements come with one main advantage over other food sources: you can maintain a consistent dose of the supplement and tailor them to your specific needs. Supplements may also help treat reproductive tract infections while addressing your gut health. As previously mentioned, speak with your doctor and our team about supplementation.
Limit or Stop Alcohol Use
Alcohol can negatively affect your gut microbiome and cause complications with fertility. It can create microbe imbalances and even overgrowth, put extra pressure on your liver, and cause inflammation, so it’s recommended to lower your consumption while trying to conceive. To keep your gut as healthy as possible, consider eliminating most alcohol from your diet.
Exercise Regularly
Frequent exercise improves blood flow and oxygen absorption, which in turn helps your gut function better. You don’t need to do heavy lifting or run several miles daily – a 30-minute session of moderate exercise that raises the heart rate is enough to help your body stay healthy. Don’t push yourself too hard, and be sure to find some physical activity that can keep you physically and mentally fit.

Reduce Stress
We know this is easier said than done; infertility struggles can be stressful enough, and other outside stresses can further complicate things. However, increased stress results in higher levels of cortisol, the stress hormone, which can cause issues in the gut microbiota. If you can find ways to reduce your stress, your gut health and fertility may improve.
Fortunately, there are plenty of strategies to consider for reducing stress:
- Exercise – Aside from its physical benefits for gut health, exercising can help reduce stress. By exercising even a small amount, your body will release endorphins that make you feel better and improve coordination.
- Meditation and Mindfulness – Meditation and mindfulness practices allow you to focus on your breathing and break away from stressful distractions, helping you remain balanced and improve your mental health. You can practice meditation or mindfulness anywhere, though we recommend a quiet environment.
- Yoga – Yoga involves stretching your body into different positions to help release tension and keep you focused on the present rather than on stressful contributors.
- Counseling – If you’re unsure how to proceed with a stressful situation or are hesitant to discuss your infertility with others, speaking with a licensed counselor or therapist may help you navigate your situation and find a way forward.
We know how challenging it can be to reduce your stress, but doing so can help you improve your chances of conception.
Get Plenty of Sleep
An adequate amount of restful sleep every night is crucial in reducing stress and maintaining proper gut health. Some people find that they sleep better after taking steps to reduce stress. Sleeping properly allows your body, including your gut, to recharge and rest. Poor sleep can cause issues with the gut microbiota, while gut issues can lead to poor sleep. Doing what you can to interrupt this cycle can help you improve your chances of conceiving.
More Gut Health Tips
Prioritizing your gut health can be an essential step in addressing your difficulty in conceiving. Still, the exact route necessary to boost your gut health to increase fertility rates is still the subject of much research. Taking simple steps to improve your diet, like eating lean proteins, plenty of fruits and vegetables, whole grains, and healthy fats while avoiding processed, high-fat, or sugary foods, is a great start. Then, add probiotic and prebiotic foods to help your microbiota flourish.
Remember: it’s essential to use caution and take your time when making any lifestyle change. Eating too many probiotic and prebiotic foods can cause an upset stomach and imbalances. Take your time and let your body slowly make adjustments.
Arizona Gynecology Consultants Can Help Address Your Infertility
For several years now, we’ve slowly begun to understand the link between fertility and gut health. Research is ongoing, and we may soon find new strategies for addressing infertility and gut health. Still, there’s a lot of information available already, and your gynecologist can help you determine whether an unhealthy gut may be contributing to your infertility struggles.
The compassionate medical team at Arizona Gynecology Consultants can help you evaluate your overall health and determine potential causes of infertility. Adjustments to your lifestyle and daily routine, including those necessary to address gut health, could help you become pregnant without the need for other interventions. For further help, view our Arizona gynecology services and schedule an appointment.
References:
- Mei, Z., & Li, D. (2022). The role of probiotics in vaginal health. Frontiers in Cellular and Infection Microbiology, 12. https://doi.org/10.3389/fcimb.2022.963868
- Viana, J. V., da Cruz, A. G., Zoellner, S. S., Silva, R., & Batista, A. L. D. (2008). Probiotic foods: consumer perception and attitudes. International Journal of Food Science & Technology, 43(9), 1577–1580. https://doi.org/10.1111/j.1365-2621.2007.01596.x
- Lundy, S. D., Vij, S. C., Rezk, A. H., Cohen, J. A., Bajic, P., & Ramasamy, R. (2020). The microbiome of the infertile male. Current Opinion in Urology, 30(3), 355–362. https://doi.org/10.1097/mou.0000000000000742
- Qi, X., Yun, C., Pang, Y., & Qiao, J. (2021). The impact of the gut microbiota on the reproductive and metabolic endocrine system. Gut Microbes, 13(1), 1894070. https://doi.org/10.1080/19490976.2021.1894070
- Harvard Health Publishing. (2019, April 19). The gut-brain connection – Harvard Health. Harvard Health; Harvard Health. https://www.health.harvard.edu/diseases-and-conditions/the-gut-brain-connection
- Monda, V., Villano, I., Messina, A., Valenzano, A., Esposito, T., Moscatelli, F., Viggiano, A., Cibelli, G., Chieffi, S., Monda, M., & Messina, G. (2017). Exercise Modifies the Gut Microbiota with Positive Health Effects. Oxidative Medicine and Cellular Longevity, 2017, 1–8. https://doi.org/10.1155/2017/3831972
- Mayo Clinic . (2021, March 18). 12 Tips to Tame Stress. Mayo Clinic; Mayo Clinic. https://www.mayoclinic.org/healthy-lifestyle/stress-management/in-depth/stress-relievers/art-20047257

Kristina Calligan is a sub-specialty nurse practitioner in Women’s Health. A native to Arizona she obtained her Bachelor of Science in nursing in 2006 at Grand Canyon University in Glendale, Arizona. Never one to stop striving and achieving all that she could, she completed two master degrees in Nursing Science and Business Administration in 2012. Ms. Calligan joined Arizona Gynecology Consultants in 2009. Prior to working at Arizona Gynecology Consultants, she worked as a nurse in labor and delivery at several local hospitals and a research coordinator in women’s health care.











 For many 13-year-old girls, self-respect may seem like a difficult concept to fully grasp let alone put into practice. There is tremendous social pressure on young girls to please others, often at the expense of one’s own time, resources, and energy. Girls who learn to focus on pleasing others at their own expense often experience difficulties with self-care later in life. A life that revolves solely around making others happy is neither tenable nor healthy in the long run.
For many 13-year-old girls, self-respect may seem like a difficult concept to fully grasp let alone put into practice. There is tremendous social pressure on young girls to please others, often at the expense of one’s own time, resources, and energy. Girls who learn to focus on pleasing others at their own expense often experience difficulties with self-care later in life. A life that revolves solely around making others happy is neither tenable nor healthy in the long run.